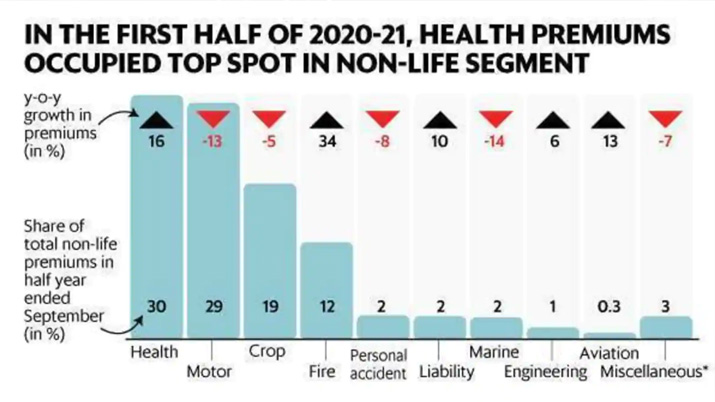
Covid-19 pandemic has made people more aware about their health and lifestyle habits. They have started adopting better lifestyles and are paying more attention towards their health. Insurers’ rising claim ratios due to the COVID-19 pandemic and new regulatory guidelines that came into effect from October 1, 2020 have pushed up premiums across the board. After the Financial Express Online published a story on February 24, 2021, drawing attention of the Insurance Regulatory Authority of India (IRDAI) towards the complaints received from the holders of health insurance policies that insurance companies have increased the renewal premium on the pretext of standardisation, the insurance regulator has asked the insurers not to modify the existing policies, that leads to increase in premiums. In a circular dated March 16, 2021, addressing CEOs of all General and Standalone Health Insurance Companies, IRDAI informed that it has added some additional norms in addition to the norms specified at Clause (C) of Chapter-III of the guidelines that general and health insurers should adhere to while effecting modification of existing products.
Several policyholders have seen their premiums at renewal shoot up 30-100 percent in some cases over the last few months. With the second wave of the deadly pandemic likely to push up claims further, insurers’ loss ratios are bound to come under pressure. “Compared to the first wave’s peak, the claim volume has increased 20-50 percent, depending on the region. It is a little early to predict the extent of premium hikes, if any, as we don’t know when the peak will come – a steady state has not yet been achieved. Insurers are in the wait-and-watch mode,” says Bhabatosh Mishra, Director of Underwriting, Products and Claims, Max Bupa.
According to some of the new norms –
- General and health insurers are not allowed to modify the existing benefits, add new benefits in the existing products, which leads to imposing an increase in premium. However, it is clarified that insurers are permitted to effect minor modifications as stipulated at Clause (G) of Chapter – III of consolidated guideline on product filing in health insurance business.
- Addition of new benefits / up-gradation of existing benefits may be offered as add-on covers or optional covers with standalone premium rate to ensure an informed choice to the policyholders.
- To simplify policy wordings, the IRDAI has asked the insurers to arrange the contents of policy contracts in a specified manner with clear heading, which is to be adopted in respect of all policies issued from October 1, 2020. The insurance regulator has also specified that customising the policy contracts of the existing products to comply with the new format will not be considered as modification.
Besides the new norms and COVID-fuelled high claim ratios, regular medical inflation and age-linked rate increases can also push up renewal premiums. Additionally, several insurance companies have, for long, adopted the practice of withdrawing existing products and replacing them with new ones with additional features, but also higher premiums. In these cases, policyholders are simply not given the option of continuing with the existing policy. However, IRDAI asked insurers to offer new benefits as add-ons or optional riders, with premiums transparently disclosed. In future, this could bring down complaints of customers having to pay more for features they never asked for.